About
Currently, a myriad of drug carriers or delivery systems have been developed to improve the overall performance and safety of therapeutic agents. However, our ability to treat neurological maladies, genetic syndromes, cancer, etc., remains a major challenge. One of the prime obstacles is our limited knowledge on the biological parameters that regulate the interaction of these systems with our tissues and, hence, our inability to gain non-invasive, efficient, and specific access within the body, its cells, and subcellular organelles.
To generate knowledge and tools to overcome this obstacle, we study the biological mechanisms ruling how our cells and tissues transport cargoes to precise destinations within our bodies and apply this knowledge to the design of nanodevices for improved delivery of therapeutic agents to specific disease sites.
Biologically-Controlled Transport of Drug Carriers
Most current strategies aim to bind a drug nanocarrier to a specific cell-surface receptor; but after said binding takes place, receptor-associated signaling and transport processes take control. Instead, our laboratory can impart a drug carrier control over the biological events that occur beyond binding. We have shown how using the same receptor, the kinetics, mechanism, and destination of a drug carrier can be modulated by: (a) varying its size, shape, and targeting valency; (b) varying the receptor epitope to which the carrier binds; (c) coupling carriers to signaling molecules; (d) combining targeting to several receptors; or (e) coupling targeting moieties with anti-phagocytic moieties on the surface of drug carriers.
Transport of Drug Carriers Across Physiological Barriers
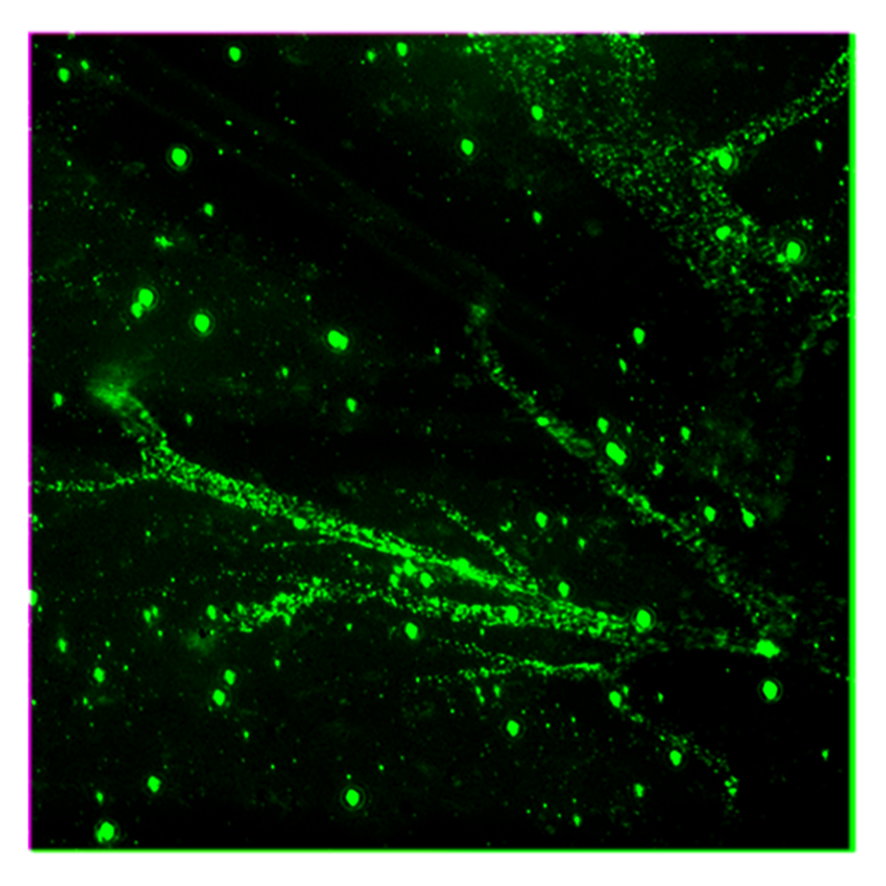
Crossing the linings that separate body and cellular compartments is paramount for efficient drug delivery. We were first to identify a natural pathway regulated by ICAM-1, a cell adhesion molecule overexpressed by most cells under pathological states, which enables transcytosis across the epithelial barrier that separates the gastrointestinal tract from the bloodstream for oral delivery, and the blood-brain barrier that separates the bloodstream from the brain tissue for delivery of therapeutics against neurological diseases. We also work with DNA-built nanocarriers which enable uptake within cells and endosomal escape for delivery to the cytosol and other subcellular compartments.
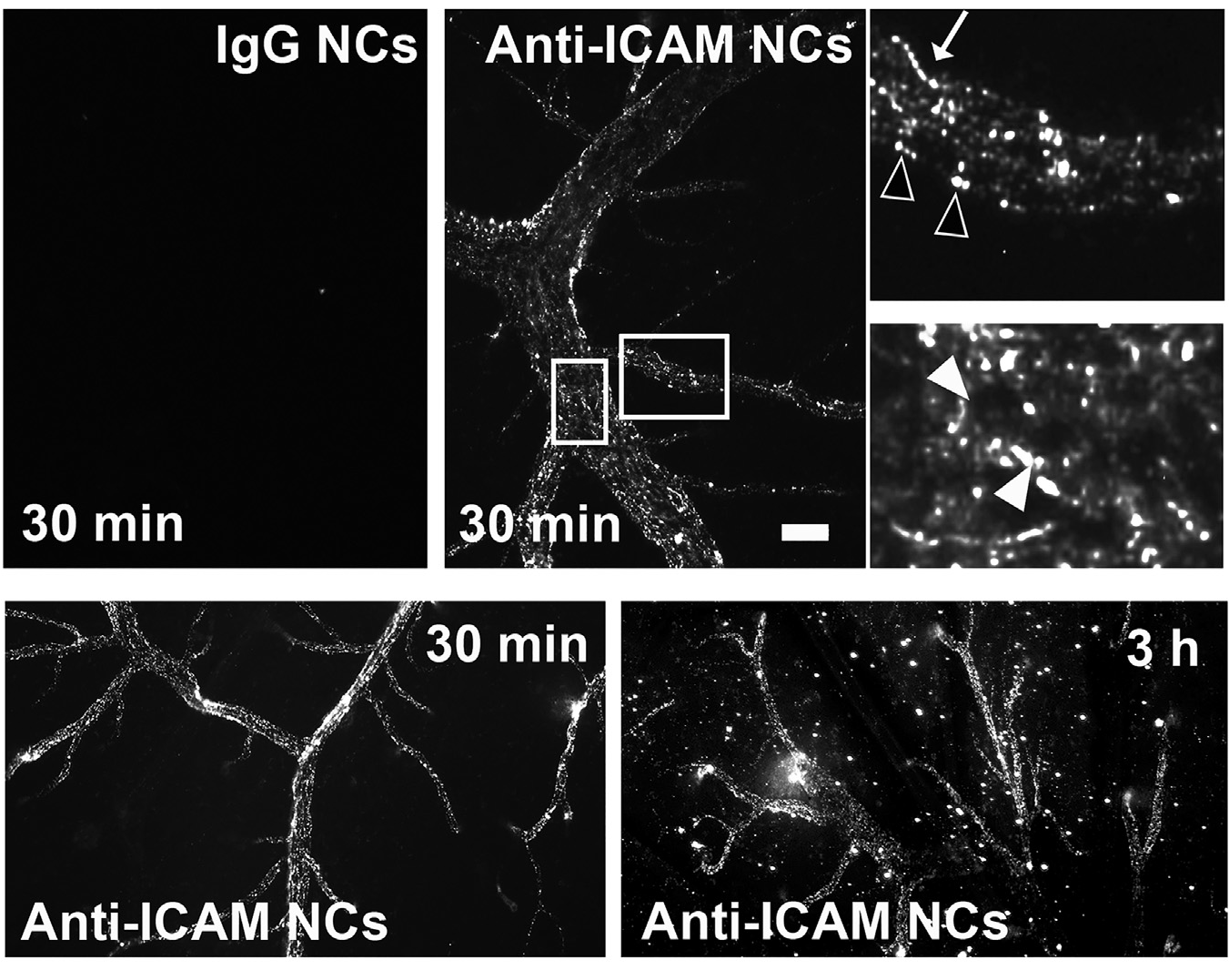
Figure 1. ICAM-1-targeted nanocarriers (anti-ICAM NCs) crossing the blood-brain barrier in an animal model. Fluorescence microscopy of cortical brain samples isolated from mice 30 min or 3 h after intravenous injection with green-fluorescent anti-ICAM NCs or control IgG NCs. Scale bar = 10 μm. Boxes = regions magnified 3-fold in the right panels. Arrows = NCs on the blood-facing surface of the blood-brain barrier. Open arrowheads = NCs on the brain-facing surface of the blood-brain barrier. Closed arrowheads = NCs inside of brain endothelial cells. Extracted from Manthe et al., Intertwined mechanisms define transport of anti-ICAM nanocarriers across the endothelium and brain delivery of a therapeutic enzyme. J Control Rel. 324 (2020):181-193).
Improving Treatment of Lysosomal Disorders
Pathologies due to monogenic deficiencies, such as the case of lysosomal disorders, are valuable models to study disease progression and therapeutic intervention because of their well-known etiology, unequivocal diagnosis, and availability regarding patient samples, diverse cell types, and animal models. Since these diseases associate to either acute or long-term effects depending on genetic severity, and they associate with neurodegeneration, cardiovascular, metabolic, and cancer-like syndromes, they represent excellent disease models. Consequently, we are applying targeted nanotechnology concepts to the treatment of genetic lysosomal disorders. Current therapies by i.v. enzyme infusion are only helpful for diseases where clearance cells and organs (liver, spleen, macrophages, etc.) are the main targets. Yet, delivery to other organs such as the brain, lungs, etc. hinders treatment for most of these diseases. Using types A and B Niemann-Pick, Fabry, and Gaucher diseases as examples, we are developing new therapeutic strategies to deliver therapeutic enzymes to all affected organs in animal models, which holds considerable translational potential.
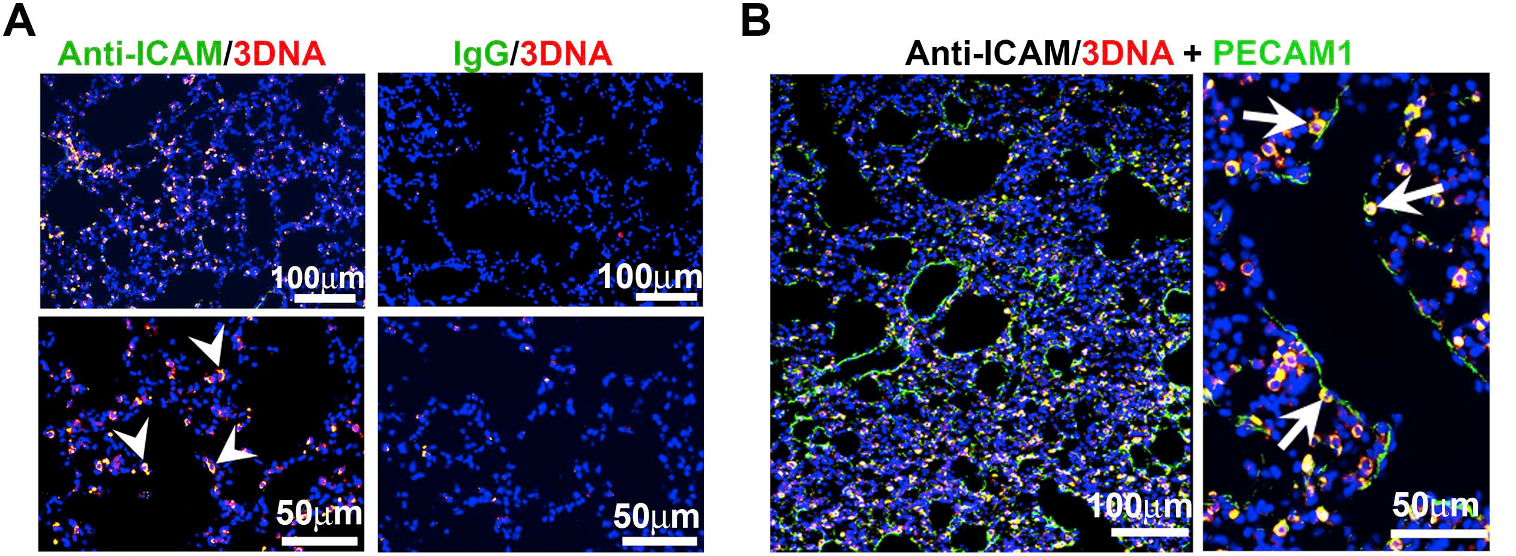
Figure 2. ICAM-1 targeted DNA-made nanocarriers (anti-ICAM/3DNA) for drug delivery to the lungs. Cy3-labeled 3DNA targeted to ICAM-1 (anti-ICAM/Cy3-3DNA) or non-targeted controls (IgG/Cy3-3DNA) were intravenously injected in mice. Lungs were isolated and processed at sacrifice at 60 min. (A) Confocal microscopy shows Cy3 3DNA (red), while the targeting coat (antibody) is visualized using a FITC-secondary antibody (green). Arrowheads show colocalization of the antibody on the coat of 3DNA. (B) Confocal microscopy showing anti-ICAM/Cy3-3DNA (red) and lung endothelial cells visualized using polyclonal anti-PECAM-1+FITC-secondary antibody (green). Arrows indicate colocalization of Cy3-3DNA with endothelial PECAM-1. (Extracted from Roki et al, Unprecedently high targeting specific to lung ICAM-1 using 3DNA nanocarriers. J Control Release. 305 (2019):41-49).
Staff
Projects
| NATIONAL PROJECTS | FINANCER | PI |
|---|---|---|
| CROSSTARGET · Desarrollo de nuevas herramientas traslacionales multi-especie para el direccionamiento de terapias con precisión de órgano y subcelular (2019 – 2022) | Ministerio de Ciencia, Innovación y Universidades | Silvia Muro |
| NANO-GBA · Assessing the effects of glucocerebrosidase (GBA) alterations on receptor membrane nanoarchitecture to design improved nanomedicines(2020 – 2021) | BIST Ignite Program | Silvia Muro |
| FUNDRAISING PROJECTS | FINANCER | PI |
|---|---|---|
| Campaña FasterFuture “A por el Parkinson” (2019 – 2021) | Fundraising | Silvia Muro |
| FINISHED PROJECTS | FINANCER | PI |
|---|---|---|
| BBB2GATE · Control diferencial del transporte de vehiculos terapeuticos dentro versus a traves de la barrera hematoencefalica (2018 – 2020) | MINECO | Silvia Muro |
Publications
Check for more detailed information on the outputs of the Group at IBEC CRIS portal.
Publications list:
Equipment
- Dynamic Light Scattering & ζ-Potential: Malvern’s Zetasizer Ultra.
Determination of the size, concentration, mobility, ζ-potential of nanoparticles, including high resolution size and MW distribution, non-invasive retrodispersion optics for wide concentration ranges, a fluorescent filter wheel to minimize artifacts from fluorescent samples, multiangle scattering (back, side, and forward scatter) to determine particle concentration without calibration, and constant current mode to measure high conductivity simples. - Gel Permeation Chromatography: Malvern’s OMNISEC.
Detector system (refraction index) of 640 nm y 50 mW, as well low (<10°) angle for highly sensitive determination of the absolute MW of polymers and proteins, upgradable to measure viscosity, branching, etc. Chromatography module, regulable pump, degasifier, sampler adaptable to many sample formats, temperature control for high MW polymers, columns/pre-columns for separation of polymers and proteins, and fraction collector. - Confocal-epifluorescence microscope: Zeiss LSM 700 microscope with 100 mW max output, 400-650 wavelength range, and IIIb class laser; 10x: EC Plan-NEOFLUAR, 20x: LD Plan-NEOFLUAR, 50x: EC Epiplan-NEOFLUAR, and 100x/1.3 oil: Plan-NEOFLUAR objectives; AxioCam Mrm camera; XLmulti S1 incubator system, and Zen 2 blue software.
Collaborations
- Dr. Alexander Andrianov, University of Maryland, MD, USA.
- Dr. Yu Chen, University of Maryland College Park, MD, USA.
- Dr. Mandy Esch, National Institutes for Standards and Technology, Gaithersburg, MD, USA.
- Dr. Robert Getts, Genisphere LLC, Hatfield, PA, USA.
- Dr. Hamid Ghandehari, University of Utah, UT, USA.
- Dr. Joe Kao, University of Maryland Baltimore, MD, USA.
- Dr. Peter Kofinas, University of Maryland College Park, MD, USA.
- Dr. Juan Marugan and Dr. Wei Zheng, National Institutes of Health, Rockville, MD, USA.
- Dr. Vladimir Muzykantov, University of Pennsylvania, Philadelphia, PA, USA.
- Dr. Gianfranco Pasut, University of Padova, Padova, Italy.
- Dr. Edward Schuchman, Mount Sinai School of Medicine, New York, NY, USA.
- Dr. Brigitte Stadler, Aarhus University, Denmark.
- Dr. Alberto Fernández de las Nieves, ICREA & University of Barcelona, Spain.
- Dr. Dolores Ledesma, CBM & CSIC, Madrid, Spain.
- Dr. Ricardo Feldman, University of Maryland, Baltimore, MD, USA.
- Dr. Ramón Farré, Clinic Hospital & University of Barcelona, Spain
- Dr. Jesús Villarrubia, Ramón y Cajal Hospital, Madrid, Spain
- Dr. Josep Samitier, IBEC & University of Barcelona, Spain.
- Dr. Giuseppe Battagglia, ICREA & IBEC, Barcelona, Spain.
- Drs. Marina Giannotti & Pau Gorostiza, IBEC & ICREA, Barcelona, Spain.
- Dr. Juana Díez, Pompeu Fabra University, Barcelona, Spain.
News
Identifiquen les millors vies per portar fàrmacs al cervell durant la malaltia de Niemann-Pick tipus A, una patologia neurològica
Investigadors identifiquen com la malaltia neurològica Niemann-Pick tipus A altera les vies naturals d’entrada de molècules al cervell i van identificar les més actives i propenses a ser utilitzades amb nanopartícules, … Read more

L’Associació Catalana per al Parkinson visita l’IBEC
El passat 18 de novembre, membres de l’Associació Catalana per al Parkinson van visitar l’Institut de Bioenginyeria de Catalunya (IBEC) per conèixer, de primera mà, el treball de Silvia Muro i el seu grup de recerca, els quals utilitzen la nanotecnologia per tractar de trobar solucions a aquesta malaltia. El treball de la professora Muro ha comptat, entre d’altres, amb el suport de les donacions rebudes a través del programa Faster Future de l’IBEC.

La campanya Faster Future contra el Parkinson culmina amb nous avenços científics
El programa IBEC Faster Future ha fet possible, durant els dos últims anys, i gràcies a les aportacions dels donants, l’estudi d’anticossos com a base d’un producte terapèutic per al tractament del Parkinson. Els investigadors presenten ara els avenços científics, i seguiran treballant per intentar donar resposta a uns dels majors reptes de la medicina moderna: les patologies neurodegeneratives com el Parkinson.

Silvia Muro, líder de grup a l’IBEC, triada per unir-se a l’elit nord-americana d’enginyeria mèdica i biològica
L’Institut Americà d’Enginyeria Mèdica i Biològica (AIMBE) ha anunciat l’elecció de la Dra. Sílvia Muro com a membre del College of Fellows pels seus èxits en el comportament de les nanomedicines a nivell cel·lular i molecular.

Investigadors de l’IBEC descobreixen una nova manera de transportar eficaçment fàrmacs al cervell
Un grup internacional d’investigadors liderats per la professora ICREA Sílvia Muro de l’Institut de Bioenginyeria de Catalunya (IBEC) i la Universitat de Maryland (Estats Units) ha descobert una nova manera de transportar fàrmacs al cervell, un dels grans desafiaments de la ciència farmacèutica actual, el que podria ajudar a dissenyar nous tractaments per a malalties neurològiques com ho són el Parkinson o l’Alzheimer. Els resultats d’aquesta investigació es recullen en un article científic publicat aquesta setmana a la prestigiosa revista Journal of Controlled Release. Per a l’elaboració del treball, els investigadors van unir un anticòs capaç de reconèixer la proteïna ICAM-1 -una molècula expressada en la superfície dels vasos sanguinis- a una sèrie de nanopartícules polimèriques capaces de transportar un fàrmac i injectar-lo per via intravenosa.
L’IBEC dedica la segona edició del programa Faster Future a la lluita contra el Parkinson
El programa IBEC Faster Future, que persegueix recaptar fons per a portar a la pràctica clínica determinats projectes que ja es troben en una etapa avançada de recerca, farà possible el desenvolupament d’un nou anticòs que serà la base d’un producte terapèutic per al tractament del Parkinson. La campanya del programa Faster Future “Pel Parkinson”, que es llança avui i que romandrà oberta fins al 30 d’abril, té per objectiu recaptar els 50.000€ necessaris per a accelerar aquesta recerca, esperant obtenir resultats favorables en un termini d’any i mig.
Jobs
Predoctoral researcher at the Targeted Therapeutics & Nanodevices Research Group (Project BRAINZYME)
Ref: FPI_SM // Deadline: 29/10/2025
Research Assistant at the Targeted Therapeutics & Nanodevices Research Group
Application Deadline: 02/12/2021Ref: RA-SM The Targeted Therapeutics and nanodevices group at the Institute for Bioengineering of Catalonia (IBEC) is looking for a Research Assistant to collaborate in a research project focused on drug delivery systems capable of targeting and crossing the blood-brain barrier (BBB) for treatment of neurological diseases involving lysosomal alterations and/or inflammation.


 ibecbarcelona.eu
ibecbarcelona.eu