 The bacterium Pseudomonas aeruginosa has great genomic plasticity that allows it to adapt to highly varied environments, and cause infections in different organs. Among them, the lungs, which are especially affected by both acute and chronic pneumonia. Its chronicity is related to its ability to enter and hide within lung epithelial cells, evading the immune system of patients and remaining latent over time, waiting for the ideal conditions to reinfect the patient, among other factors.
The bacterium Pseudomonas aeruginosa has great genomic plasticity that allows it to adapt to highly varied environments, and cause infections in different organs. Among them, the lungs, which are especially affected by both acute and chronic pneumonia. Its chronicity is related to its ability to enter and hide within lung epithelial cells, evading the immune system of patients and remaining latent over time, waiting for the ideal conditions to reinfect the patient, among other factors.
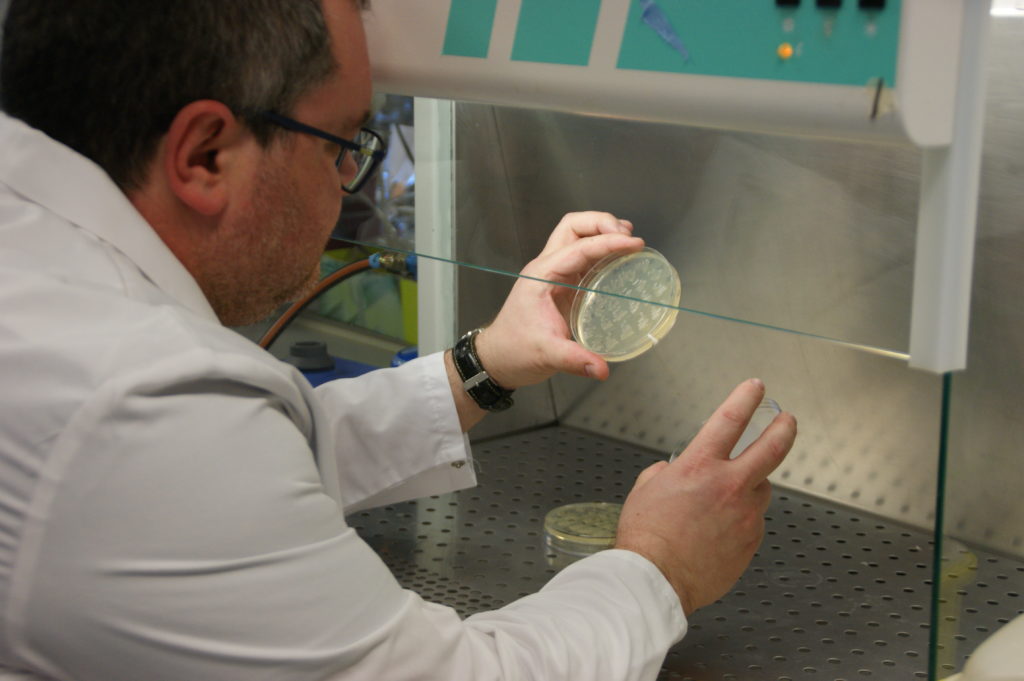
Now, a study led by Dr. Eduard Torrents, principal investigator at IBEC and professor at the University of Barcelona in the Department of Genetics, Microbiology and Statistics, and Dr. Maria del Mar Cendra, who is also a researcher at IBEC, have found variations in the ability to effectively carry out intracellular invasion between different strains of the bacterium. “We have detected differences in persistence within the cell between laboratory strains and other strains from sputum of cystic fibrosis patients and also according to the type of infected epithelial cell: alveolar, bronchial or affected by the mutation found in patients with cystic fibrosis”, explains Dr. Torrents.
The clinical P. aeruginosa strains used in the IBEC study had a greater capacity for invasion and persistence than those of laboratory strains. These differences indicate that laboratory strains are not good models for replicating bacterial infections in vivo. “The bacteria are very versatile and adapt very quickly to the environment. Therefore, it is very important to use suitable strains to study specific phenotypes. If not, the results may not be extrapolated. There are more and more studies using clinical strains to study infective models.”
With this work, published in the prestigious medical journal Virulence, the researchers have also identified a mechanism that could allow us to understand why some strains are more capable of surviving intracellularly than others. Dr. Torrents comments: “We have detected that the class II ribonucleotide reductase (RNR) enzyme is highly expressed in these persistent conditions. Therefore, it plays a critical role in maintaining the viability of P. aeruginosa during its intracellular period”. This enzyme provides the bacteria with the deoxyribonucleotides required to replicate and survive within lung epithelial cells, causing recurring infections that aggravate, for example, diseases such as cystic fibrosis and chronic obstructive pulmonary disease (COPD).
This discovery could help develop medications to prevent recurrences of lung infections. “A drug against this new antimicrobial target, RNR class II, could be helpful in inhibiting the bacterium during its intracellular persistence,” explains Dr. Torrents. “Also, since humans don’t have this enzyme, it would be very selective therapy, which is very good.”
On the other hand, this therapeutic approach could be useful for infections caused by P. aeruginosa in other organs: “Recently in our laboratory we have seen that class II RNR is highly expressed during biofilm formation. This leads us to think that it might not be restricted to the lung infections caused by this bacteria when it infects intracellularly”.
It remains to be seen if a hypothetical drug against the enzyme could be used to fight other intracellular infections. “The world of RNRs is very complex, not all bacteria express the same RNRs and those that do tend to vary greatly in sequence and structure. Depending on the mechanism of action of the drug and if the bacteria in question share the expression of this RNR, perhaps it could be possible to develop therapies against other pathogens”, concludes Dr. Torrents.
Reference article: Maria del Mar Cendra and Eduard Torrents. “Differential adaptability between reference strains and clinical isolates of Pseudomonas aeruginosa into the lung epithelium intracellular lifestyle”. Virulence, 2020
For more information and request of an interview with the researchers, please contact: alopez@ibecbarcelona.eu





