The Micro Immune Response On chip (MIRO) allows tumours and their environment to be replicated in order to understand their response to immunotherapy-based treatments. The device, which has already been successfully tested on breast cancer samples, could be key to developing new treatments and determining the most appropriate therapy for each patient in a personalized way. The work, published in Nature Communications, is the result of a collaboration between the Institute for Bioengineering of Catalonia and the Research Institute of the Hospital del Mar.
A team led by the Institute for Bioengineering of Catalonia (IBEC) and the Hospital del Mar Research Institute has developed the MIRO (Micro Immune Response On chip), a device that allows to replicate the characteristics of tumours and their environment using patient cells. It is a tool that can help speed up the development of new cancer therapy treatments as well as select the most suitable ones for each person. The work has been published in the journal Nature Communications.
MIRO enables to recreate not only the tumour, but its environment and the interaction they have with the cells of the immune system. This relationship is vital for the success of immunotherapy-based treatments.
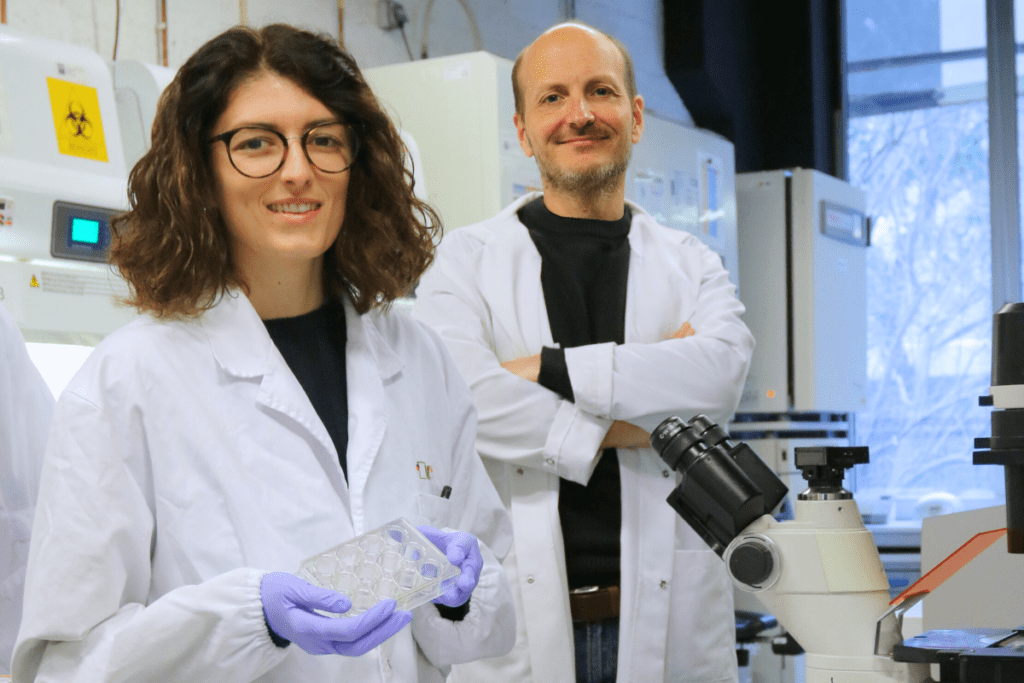
Anne Labernadie
The MIRO device makes it possible to fill a gap in the creation of treatments against cancer cells. Many developments offer promising results in the laboratory, in vitro and in mouse models, but they do not work as well when transferred to humans. “MIRO enables to recreate not only the tumour, but its environment and the interaction they have with the cells of the immune system. This relationship is vital for the success of immunotherapy-based treatments which, despite their curative potential, currently only work in between 20 and 40% of patients” explains Dr Anna Labernadie who designed the microfluidic system during her postdoctoral research at IBEC and now leads the Cell Behavior and Tissue Bioengineering laboratory at the Príncipe Felipe Research Center (CIPF) in Valencia.
The researchers who have developed this technology have already tested it with breast cancer samples known as HER2-positive. This type of cancer cell has very high levels of the HER2 protein, which promotes rapid tumour growth, but at the same time, can be treated with therapies that specifically target this protein.
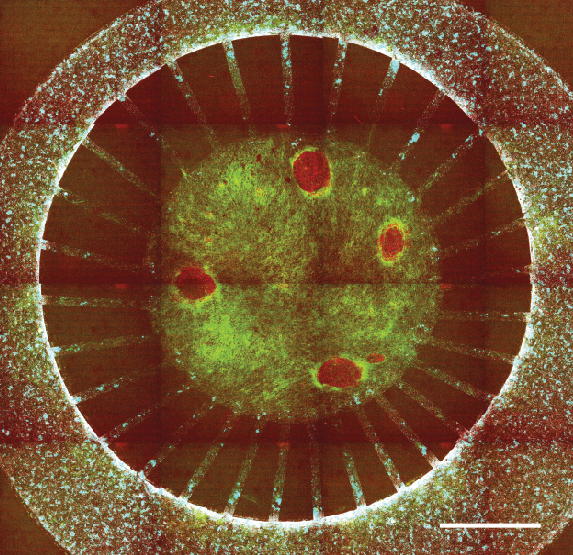
The tests carried out have made it possible to verify the importance of the environment surrounding breast tumours in protecting them from the most common treatment in this type of cancer, the monoclonal antibody trastuzumab. “Thanks to MIRO, we have been able to track the immune cells, see how they lose speed, movement, as they approach the tumour, which makes the treatment not work. They encounter a barrier formed by the tumour environment and become blocked”, explains Dr Alexandre Calon, head of the Translational Research Laboratory in Tumour Microenvironment at the Hospital del Mar Research Institute.
Moving towards personalised treatment
The MIRO device, which has already been tested with other types of solid tumours, such as lung or colon tumours, is manufactured using microfluidic techniques. These techniques allow fluids and cells to be manipulated on a very small scale. MIRO includes cell cultures of different types, separated into compartments in order to direct and observe their evolution. This model, the first of its kind created with these techniques, makes it possible to recreate and study in detail the interaction between cancer cells, their connective tissue and immune responses. “This model allows us to directly test the treatments that would be used with patients,” explains Dr Xavier Trepat, ICREA research professor at IBEC, where he leads the Integrative Cell and Tissue Dynamics group, and member of the University of Barcelona (UB).
This model allows us to directly test the treatments that would be used with patients.
Xavier Trepat
The device’s ability to analyse the functioning of different treatments, the emergence of possible resistance and even identify new biomarkers individually for each patient, represents a great advance in the design and personalisation of immunotherapy treatments in oncology.
In this sense, Dr Joan Albanell, head of the Medical Oncology Service at Hospital del Mar and director of the Cancer Research Program at his research institute, pointed out that “MIRO is an innovative preclinical model that can help improve the success rate and efficacy of new strategies with immunotherapy once we transfer them to clinical trials”.
As for future work, IBEC, ICREA and Hospital del Mar Research Institute have already filed a joint patent application for MIRO’s technology. “Our goal is to transfer this technology to the pharmaceutical industry and hospitals to be able to apply it to patients,” explains Dr Anna Labernadie.
The study described is part of Alice Preucca’s PhD thesis at IBEC. Her work focuses on investigating the role of the immunocompetent ecosystem in cancer progression.
The work also included the collaboration of the Institute for Research in Biomedicine (IRB Barcelona), the University of Barcelona (UB), the Bioengineering, Biomaterials and Nanomedicine Networking Biomedical Research Centre (CIBER-BBN), Pompeu Fabra University and the Oncology Networking Biomedical Research Centre (CIBERONC-ISCIII); and has received partial funding from the “la Caixa” Foundation.
Reference article
Alice Perucca, Andrea Gómez Llonin, Oriol Mañe Benach, Clement Hallopeau, Elisa I. Rivas, Jenniffer Linares, Marta Garrido, Anna Sallent-Aragay, Tom Golde, Julien Colombelli, Eleni Dalaka, Judith Linacero, Marina Cazorla, Teresa Galan, Jordi Pastor Viel, Xavier Badenas, Alba Recort-Bascuas, Laura Comerma, Patricia Fernandez-Nogueira, Ana Rovira, Pere Roca-Cusachs, Joan Albanell, Xavier Trepat, Alexandre Calon and Anna Labernadie. Micro Immune Response On-chip (MIRO) models the tumour-stroma interface for immunotherapy testing. Nature Communications (2025). DOI: 10.1038/s41467-025-56275-1





