Associate researcher: Jordi Alcaraz (jalcaraz@ub.edu)
Co-supervisor: Joan Montero/Josep Samitier
Lung cancer is the first cause of cancer death in developed countries, with a 5-year survival rate of ~18%. Promising therapeutic results have been recently obtained with immune checkpoint inhibitors (ICIs) like PD-L1 blocking antibodies, which remove the breaks against the immune system of those lung cancer cells that overexpress PD-L1 and ultimately boost antitumor immune responses. However, positive responses to ICIs are still limited to a reduced number of patients, suggesting the existence of immune evasive processes other than PD-L1 overexpression. In addition to cancer cells, it is increasingly recognized that the surrounding desmoplastic stroma rich in activated fibroblasts (TAFs) plays a key role in both tumor progression and resistance to ICIs therapies, owing to their strong immunosuppressive properties.
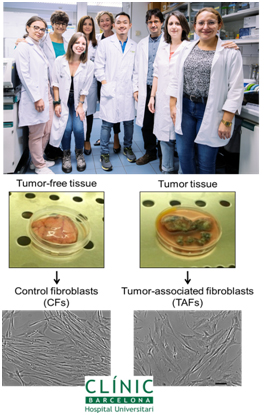
The goal of this project is to first identify the major immunosuppressive processes of TAFs in lung cancer, and to screen for effective drugs that prevent such processes, therefore potentially enhancing current responses to ICIs. For this purpose, the PhD candidate will benefit from our collection of patient-derived TAFs (unique in Spain and one of the fewly available worldwide) (Puig et al, Mol Cancer Res 2015), in vivo models (Lugo et al, Carcinogenesis 2016), and new preclinical models based on culturing ex-vivo precision cut fresh tumor samples from surgical patients (Marin et al, J Thor Oncol 2019).
 This translational project will be carried out in close collaboration with oncologists at the Hospital Clínic, which is the leading clinical institution in Spain in terms of scientific productivity. As part of this collaboration, this project will include the participation in the monthly meetings of the new Functional Unit of Thoracic Tumors at the Hospital Clínic with oncologists, pathologists, radiologists, surgeons, neumologists and translational biomedical scientists like us. Moreover, this project will be pursued in collaboration with pharmaceutical companies that are developing new drugs against the aberrant stroma rich in activated TAFs (Ikemori et al, Cancer Res 2020; Gabasa et al, Brit J Cancer 2017). Experimental tools will also include the state-of-the-art of molecular and cell biology techniques as well as bioengineering approaches to improve our new ex-vivo model. The positive results from this project will be instrumental to facilitate the development of clinical trials combining ICIs with anti-stromal drugs.
This translational project will be carried out in close collaboration with oncologists at the Hospital Clínic, which is the leading clinical institution in Spain in terms of scientific productivity. As part of this collaboration, this project will include the participation in the monthly meetings of the new Functional Unit of Thoracic Tumors at the Hospital Clínic with oncologists, pathologists, radiologists, surgeons, neumologists and translational biomedical scientists like us. Moreover, this project will be pursued in collaboration with pharmaceutical companies that are developing new drugs against the aberrant stroma rich in activated TAFs (Ikemori et al, Cancer Res 2020; Gabasa et al, Brit J Cancer 2017). Experimental tools will also include the state-of-the-art of molecular and cell biology techniques as well as bioengineering approaches to improve our new ex-vivo model. The positive results from this project will be instrumental to facilitate the development of clinical trials combining ICIs with anti-stromal drugs.

