Researchers identified how a neurological disease from the group of the lysosomal storage disorders, alters the natural entrance routes of molecules in the brain. They identified the most active ways prone to be used by nanoparticles capable of delivering therapeutical drugs.
These findings open the door to improve existing treatments for neurological diseases, and to develop new ones, based on nanoparticles being used as “Trojan horses” to bring drugs inside the brain trough the identified routes.
The blood-brain barrier protects the brain from the entrance of toxic molecules, but in the same way, it also hinders brain penetration and therapeutic effects of most drugs. Many strategies have been attempted to overcome this barrier, but they have not been successful regarding the transport of big molecules such as enzymes and other proteins.
Researchers from the Institute for Bioengineering of Catalonia (IBEC) in collaboration with the Institute for Bioscience and Biotechnology Research, University of Maryland in the USA, have now observed how a neurological disease alters the natural routes of transport between the circulation and the brain. By examining three of these routes, they identified which of the routes are more active to then design nanoparticles capable of delivering therapeutics into the brain. The findings were recently published in the Journal of Controlled Release.
Crossing the blood-brain barrier during disease
Delivery of therapeutics into the brain remains a formidable challenge because of the presence of the blood-brain barrier, a cellular structure that separates the circulation from this organ to protect it from toxic substances. Nanomedicine is finding ways to exploit natural transport routes across this barrier, but how these routes are affected during disease is unknown, which hinders our ability to design efficient treatments for neurological diseases.
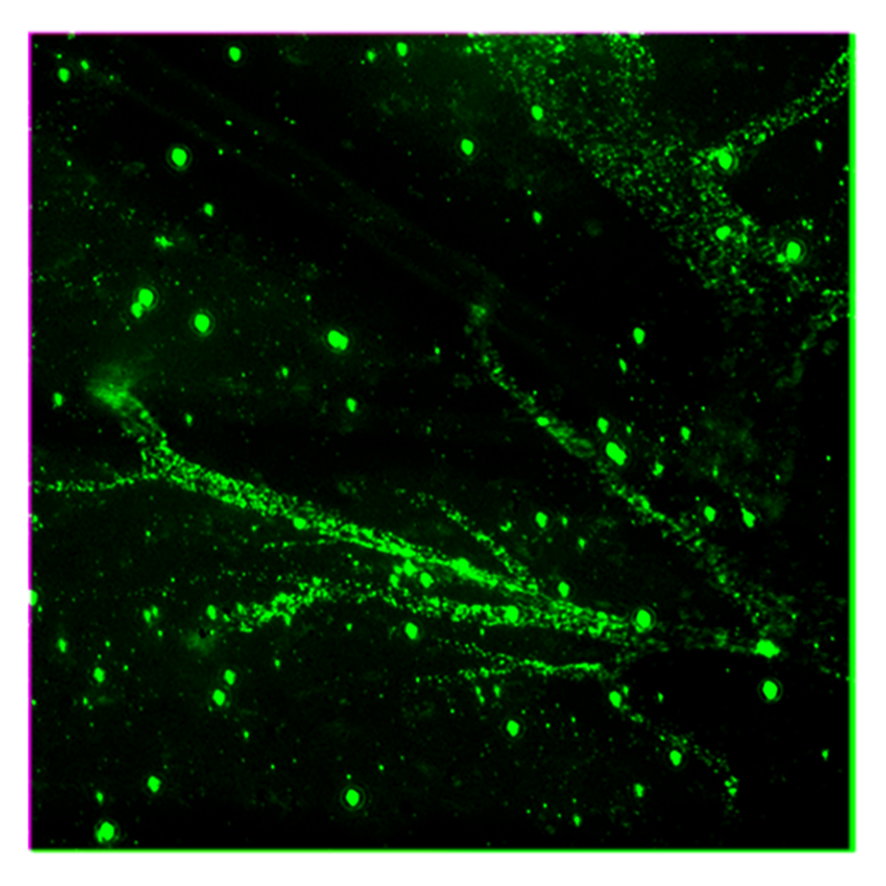
In this study, researchers focused on a transport mechanism known as transcytosis, where a molecule crosses the blood-brain barrier passing through its endothelial cells, the protective cell layer around the brain. The objective is to exploit this transcellular transport to elicit effective delivery of a therapeutic cargo into the brain. Researchers analysed how a neurological disease influences the transcytosis routes associated with three different pathways to identify the best ones to be used for treatment.
Specifically, they focused on Niemann Pick disease type A, a currently untreatable disease that appears in new-borns and infants, in which an abnormal lipid metabolism leads to its accumulation on vital organs as liver, lungs, and mainly brain. Patients develop at abnormal rates and have their nervous system gradually deteriorated, leading to high mortality.
Niemann Pick disease is included in a group of more than 60 inherited metabolic disorders called lysosomal storage disorders (LSD). There is no current treatment for majority of these diseases, which cause patients to die within months or few years of life. In addition, some of these defects are known to be associated with common and chronic neurological diseases such as Parkinson’s, which affects more than 10 million people worldwide and costs 52 thousand million dollars in the US alone, 10.000-20.000 € per patient-year in Europe.
“The suitable routes identified and nanotechnology platforms designed to exploit them offer a new opportunity to reformulate therapeutics previously unable to enter the brain for the treatment of these conditions”.
Silvia Muro (IBEC), lead researcher of the study.
Lysosomes are known as the “recycling bins” of cells in our body, including neurons, as their main function is to processes unwanted material into substances that the cell can use or disposed of, by breaking and modifying them with enzymes. If one or more enzymes are defective (due to gene mutations), excess products destined for breakdown and recycling accumulate in the cell in a deleterious manner.
By applying leading techniques as confocal microscopy, radiotracing and nanotechnology to analyse postmortem brain tissue from patients and animal models, as well as cellular models of the blood-brain barrier, researchers could identify which of the three routes examined was altered by disease and select the best route to transport molecules into the across the blood-brain barrier during this disease.
Nanocarriers to shuttle drugs
The identification of the best routes to cross the BBB during a neurological disease supports the development of drug delivery approaches to elicit macromolecular transcytosis across the blood-brain barrier. Nanocarriers are useful tools in this regard and can be used in a molecular Trojan horse strategy, as they can be loaded with a variety of therapeutic cargoes or drug combinations and protect them from the systemic environment.
Effective design of nanocarriers for therapeutic brain targeting can guide future therapeutic interventions for the treatment of Niemann-Pick disease type A, other LSDs, and could be easily extended to the treatment of Alzheimer’s and Parkinson’s diseases.
Reference article: Melani Solomon, Maximilian Loeck, Marcelle Silva-Abreau, Ronaldo Moscoso, Ronelle Bautista, Marco Vigo, Silvia Muro. Altered blood-brain barrier transport of nanotherapeutics in lysosomal storage diseases. Journal of Controlled Release





