Chronic wounds are a challenge for microbiologists due to biofilms, complex structures where bacteria protect themselves from antibiotics, preventing infections from being treated effectively. A research team led by the Institute of Bioengineering of Catalonia (IBEC) has published in the journal Frontiers in Microbiology a study on how the use of specific enzymes and the combination of different antibiotic drugs can mean a breakthrough in the fight against this problem.
The chronicity of wounds is a relevant health problem affecting almost 2 million people in Europe. The primary cause of these wounds not healing is the presence of polymicrobial communities that form an extracellular matrix that protects them from antimicrobial agents and cells of our immune system giving rise to a three-dimensional organization known as a biofilm.
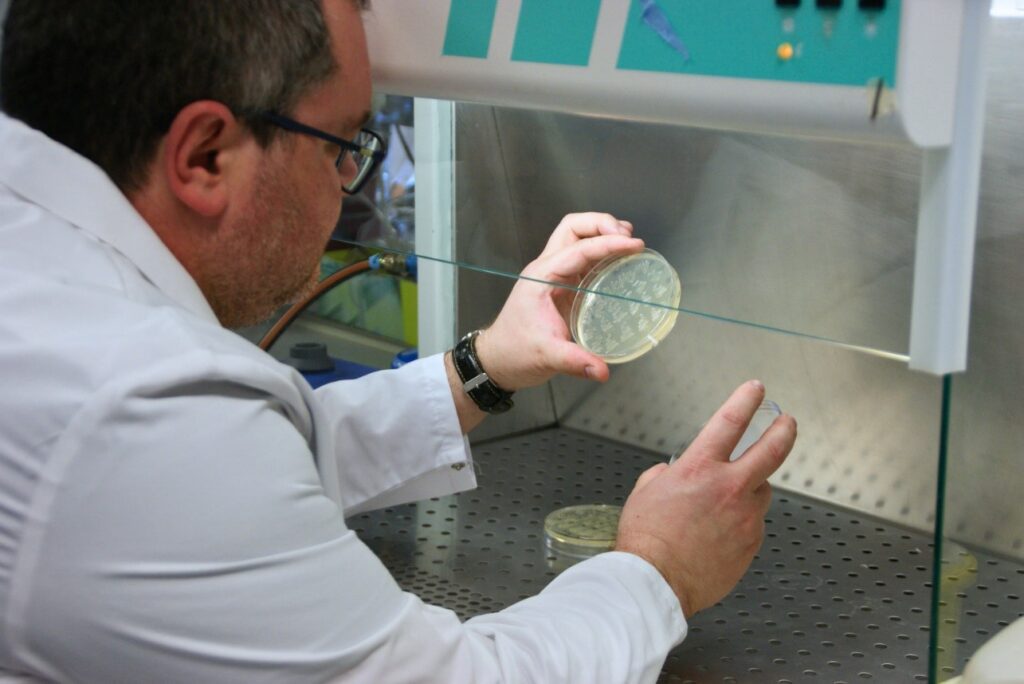
A study led by Alba Rubio Canalejas, an IBEC researcher, and Eduard Torrents, a researcher at IBEC and the University of Barcelona, in collaboration with the Jozef Stefan Institute in Slovenia, describes the design of an innovative treatment based on the use of optimized silver nanoparticles with enzymes and two combined antibiotics, which is highly effective against biofilms. The research, published in Frontiers in Microbiology, deals specifically with biofilms produced by dual infection of bacteria Pseudomonas aeruginosa y Staphylococcus aureus, two very usual microorganisms in this type of wounds.
Enzymes and antibiotics combined against microbial biofilms
Biofilms are structures formed by pathogenic bacteria and a matrix that surrounds them, made of polysaccharides, proteins, lipids, and extracellular DNA, which hinder the diffusion of antibiotics and prevent the wound from treatment.
“It is necessary to investigate therapies that improve the penetrability and efficacy of antimicrobials in this situation,” explains Torrents. “Silver, for example, is known to have antimicrobial properties. We decided to use silver nanoparticles, optimized with different enzymes, to see which ones were most effective at breaking down the matrix that makes up P. aeruginosa and S. aureus”. The researchers demonstrated that treatment with silver nanoparticles optimized with the enzyme DNAsa I reduced the multiplying capacity of P. aeruginosa by 99.98% and that of S. aureus by 92.3% in an in vitro wound model.
Once the matrix was opened, using more than one antibiotic at a time proved to be crucial in ending the infection. According to Rubio-Canalejas, “these two bacteria have a complex relationship in nature, where they can be competitive, due to the exoproducts produced by P. aeruginosa that suppress the growth of S. aureus. However, in the context of biofilms, they establish synergies and collaborate. The dual infection increases their resistance and tolerance to antimicrobials, allowing them to colonize tissue and prevent wound healing.” The researchers found that using a single type of drug affected each species of bacteria differently. The antibiotic ciprofloxacin caused P. aeruginosa to outperform S. aureus, and gentamicin caused the opposite effect. However, a dual therapy that combined both compounds reduced the populations of both species.
“There is very little literature on how bacteria are distributed within polymicrobial biofilms. Figuring out how they organize themselves can go a long way toward improving future treatments.”
Eduard Torrents
Moreover, the researchers studied the internal composition of the biofilm, representing, for the first time, a general scheme of how bacteria are distributed in three-dimensional space. “We saw that S. aureus forms aggregates in the innermost part of the biofilm, thus protecting itself from P. aeruginosa. This allows both to coexist and worsen any infection,” explains Torrents.
In conclusion, the study opens a new avenue to comprehend biofilms and design clinical treatments that combine enzymes and antibiotics and are essential to eliminate infections in chronic wounds.
Reference article:
Alba Rubio-Canalejas, Aida Baelo, Sara Herbera, Núria Blanco-Cabra, Marija Vukomanovic y Eduard Torrents. 3D spatial organización and improved antibiotic treatment of a Pseudomonas aeruginosa–Staphylococcus aureus wound biofilm by nanoparticle enzime delivery. DOI: https://doi.org/10.3389/fmicb.2022.959156





